What Are Portable Benefits and How Does it Impact Your Business
July 26, 2024
The Key Challenges SMEs Face with Traditional Healthcare Administration
September 11, 2024Protect Your Bottom Line: Mednefits’ Strategies to Prevent Benefits Abuse
Employee Benefits
Protect Your Bottom Line: Mednefits' Strategies to Prevent Benefits Abuse
4 September, 2024
In the ever-evolving landscape of employee benefits, organisations face a significant challenge: benefits abuse. This issue not only threatens the financial viability of benefits plans but can also lead to increased premiums, diminished coverage, and strained employee relations. At Mednefits, we recognise the importance of maintaining the integrity of your benefits programme. This article explores comprehensive strategies to prevent benefits abuse, ensuring that your organisation protects its bottom line while fostering a culture of accountability and trust.
Understanding Benefits Abuse
Benefits abuse refers to the misuse of health benefits for personal gain, often manifesting as fraudulent claims or excessive utilization of services. This abuse can take various forms, including:
Fraudulent Claims:Employees may submit claims for services that were never rendered or misrepresent medical conditions to obtain benefits or medical certificates (MCs) they are not entitled to.
Overutilisation of Services:Some employees might exploit their benefits by seeking unnecessary medical treatments or services, leading to inflated costs for the organisation.
MC Abuse:Employers may notice a rise in employee medical certificate (MC) submissions which may impact overall healthcare costs and productivity as well as affecting the way HR verifies the accuracy of these submissions. This may, in turn, pose more complexities in pinpointing the reason behind the cost increase.
The Financial Impact of Benefits Abuse
The financial repercussions of benefits abuse can be staggering. According to industry estimates, fraud and abuse can account for 3% to 10% of total healthcare spending. This strains the financial resources of an organisation and can result in higher claims costs. To offset the costs associated with abuse, employers may also be forced to reduce benefits or increase employees’ out-of-pocket expenses.
How do we combat this?
- Implement strong monitoring systems
Establishing robust monitoring systems is essential for detecting and preventing benefits abuse. Mednefits provides tools that allow employers to track benefits usage in real-time, identifying unusual patterns or discrepancies. This proactive approach helps catch potential abuse early. Mednefits also utilises advanced analytics to identify trends and anomalies in claims data, allowing organisations to pinpoint areas of concern and address them before they escalate.
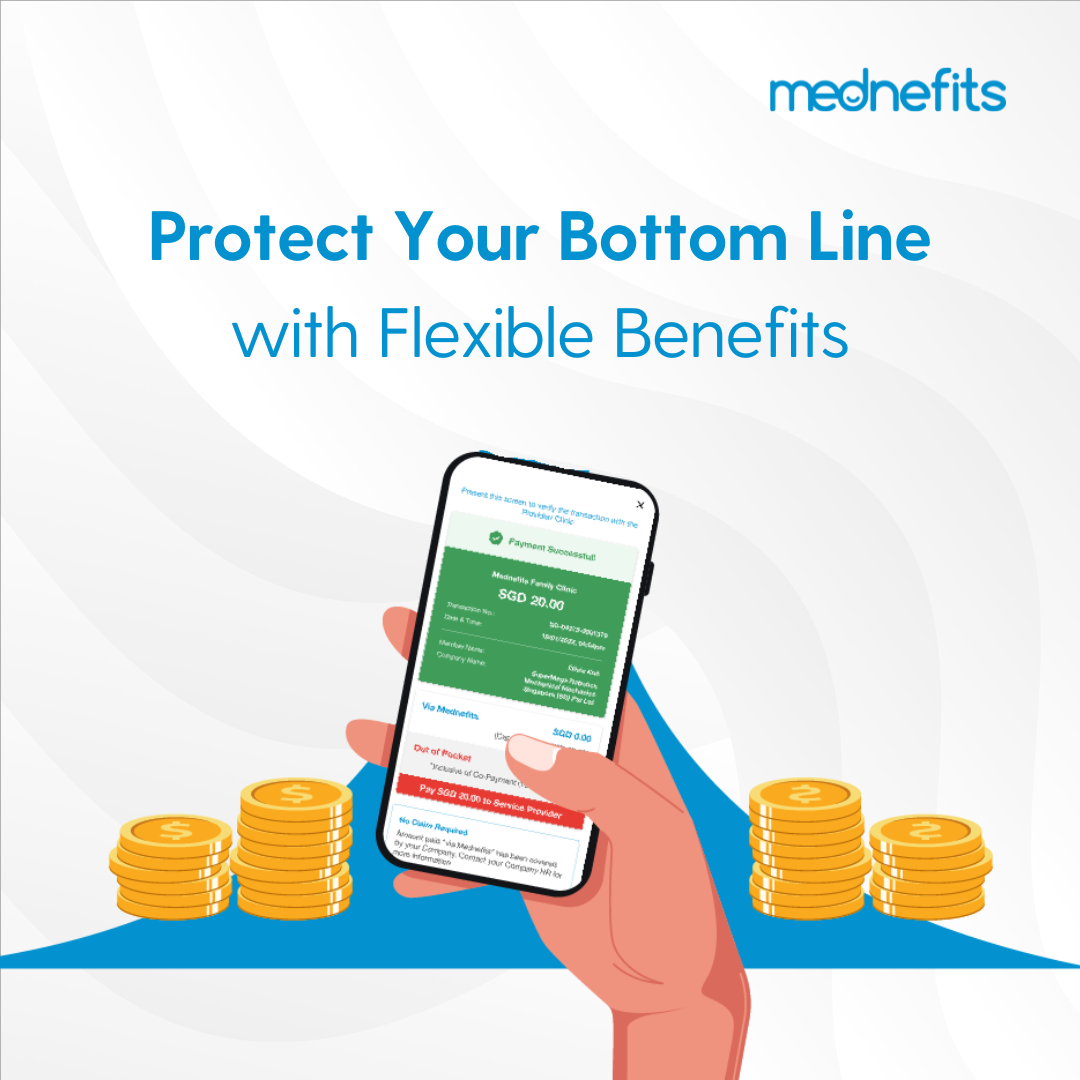
- Utilise technology for enhanced security
In an increasingly digital world, utilising technology can bolster defenses against benefits abuse. Mednefits provides a platform that ensures sensitive information is protected through multi-factor authentication and data protection certified by ISO. Mednefits also keeps employees informed about their claims and any suspicious activities through automated notifications, reducing the chances of fraudulent claims going unnoticed.
- Collaborate with Benefits Providers
Partnering with a reputable benefits provider is crucial for maintaining the integrity of your benefits plan and ensuring there are systems in place to prevent benefits and MC abuse. Mednefits’ user-friendly platform instantly validates the MCs in real-time as well as electronically matches MCs to clinic visits for verification. The platform also offers preventive capabilities such as visit caps and customised employee panel access to aid in curbing any potential benefits abuse. These systems should be in place to aid in developing effective policies to prevent and address benefits and MC abuse.
Investing in these strategies not only protects your benefits plan but also fosters a culture of integrity and accountability within your organisation. With Mednefits, you can navigate the complexities of employee benefits with confidence and security, ensuring that your organization thrives in a competitive landscape while providing valuable support to your employees.